Using the PELI to Advocate for Person-Centered Care
Have you heard the term person-centered care but you aren’t sure exactly what it means? Would you like to learn new ways to get to know the individuals under your guardianship? Would you like to advocate for them by suggesting specific practical steps that providers can take to offer better care?
A Special Toolkit for Guardians and Advocates
This toolkit introduces guardians and advocates to the concept of person-centered care and then describes a three-step process to advocate for improved quality of care for older adults receiving long-term services and supports. The three steps are:
- Step 1: Assess an Individual’s Preferences with the Preferences for Everyday Living Inventory (PELI)
- Step 2: Incorporate Preferences into Care Plans
- Step 3: Communicate Preferences to Enhance Person-Centered Care
The toolkit also touches on strategies to handle preferences that involve risk, and ways to learn about preferences when a person cannot communicate through words as well as other key topics. Three appendices provide additional guidance on pages 6- 10. All resources mentioned in the toolkit are available for free download at PreferenceBasedLiving.com.
What is Person-Centered Care?
According to the Centers for Medicare and Medicaid Services (CMS), person-centered care (PCC) means:
Simply put, person-centered care means “knowing the person” and honoring their individual preferences.
Making an effort to understand what each resident is communicating, verbally and nonverbally; identifying what is important to each resident with regard to daily routines and preferred activities; and having an understanding of the resident’s life before coming to reside in the nursing home.
Assessing and honoring everyday preferences is a foundation for person-centered care. When preferences are understood and honored, each person has a greater sense of autonomy, quality of life, and emotional wellbeing. Furthermore, care team members who know a person’s preferences can anticipate their needs and work more efficiently, spending time where they have the greatest impact. Honoring preferences helps those receiving care to maintain authorship of their own lives.
What is the PELI Questionnaire and Where can I Find It?
The Preferences for Everyday Living Inventory (PELI) is a scientifically validated questionnaire that helps you learn about a person’s most important preferences. Phrased in clear, conversational language and tested with a wide variety of older adults, the PELI gathers practical information about how each person likes to live daily life – the time they prefer to wake up and get dressed, whether to take a shower or bath, and the recreational activities that bring the most pleasure.
Guardians and advocates can use the PELI to guide one-on-one conversations with individuals under your care – and as a framework for discussions with direct care workers and other team members. The PELI enables you to get to know older adults – as well as the staff who work with them every day — in order to build insight, relationships, mutual respect, and trust that will result in better and more personalized care.
The PELI was developed as a public service to assist health care providers in delivering person-centered care. It is based on extensive research generously supported by the federal government and multiple foundations. For more information about how the toolwas developed and tested, see our tip sheet “What is the PELI?,”which can be found on the Resources page of our website. PELI questionnaires, tip sheets, training videos and related resources are available for free download at PreferenceBasedLiving.com.
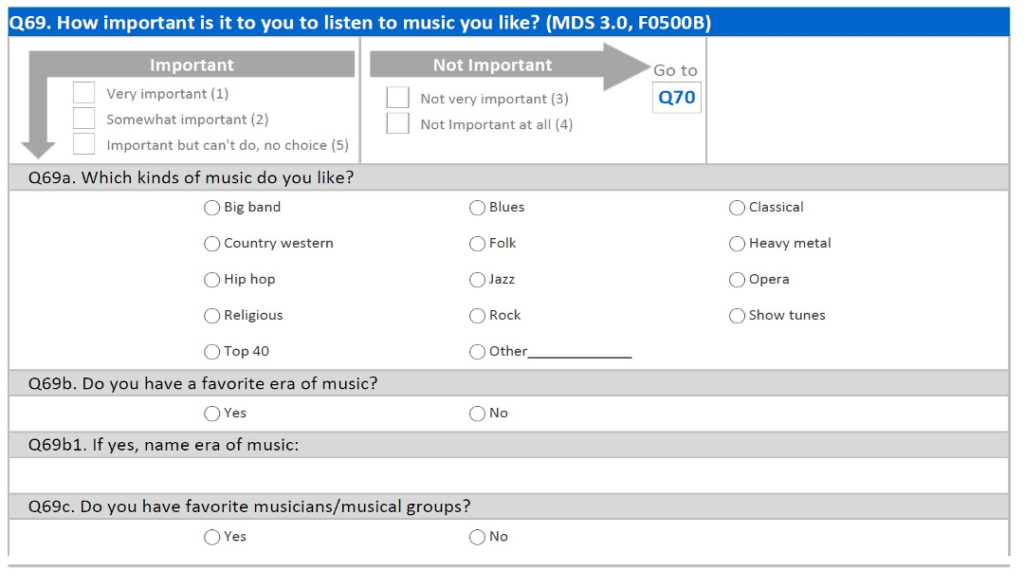
PREFERENCES FOR EVERYDAY LIVING INVENTORY – SAMPLE
Step 1: Assess Important Preferences for Everyday Living
Before you begin using the PELI to interview older adults, we recommend that you review tips on Assessing and Individual’s Important Preferences in Appendix A (page 6) of this toolkit, and view our brief video on Interviewing Older Adults Using the PELI. Also, think through the goals of your interview and whether it’s best to ask the full PELI’s 72 questions, or concentrate on a smaller subset of preferences. The PELI is a flexible tool that comes in four versions. Consider these options for your interview:
When you’d like to get to know about the complete range of a person’s preferences for daily living, use the PELI–Nursing Home–Full questionnaire. This version asks about 72 different preferences, but guardians and advocates can choose which items to focus on.
- Keep in mind: You do not need to ask all 72 questions in one sitting. As time is often limited and individuals may become fatigued, it’s okay to do a few PELI questions at a time.
- For all older adults, and particularly those from the Lesbian, Gay, Bisexual and Transgender community, use the 72-item Rainbow PELI, which includes specially tailored follow-up questions similar to the Nursing Home-Full version.
- For a shorter interview that gathers additional details for 16 preferences that may have already been assessed, use the PELI–Nursing Home–MDS 3.0 Section F.Ask the provider for a copy of the federal Minimum Data Set (MDS) 3.0 Section F –Routine Preferences assessment, which is part of each nursing home resident’s medical record and covers 16 preferences. Visit with the individual and review their MDS responses together. For preferences marked “Very Important,” “Somewhat Important,” or “Important, But Can’t Do,” ask the supplemental questions found in the PELI–Nursing Home–MDS 3.0 Section F questionnaire.
- If time is limited and you want to refine the scope of the interview, review the PELI-Nursing Home-Full version to select topics most relevant for the individual under guardianship. Each question is a standalone item, which allows you to pick and choose those that are most appropriate for each person.
- If you are looking for a starting point to narrow down the questions, use the PELI-NH-Full questionnaire but focus only on the “top ten” preferences of older adults using long-term services and supports. Our tip sheet, Top Ten Preferences Across LTSS Settings, provides background on these popular preferences:
| “TOP 10” PREFERENCES* | PELI QUESTION AND PAGE NUMBER |
| Choosing the time to bathe or shower | Q 05, page 2 |
| Having privacy | Q 32, page 15 |
| Choosing what to eat | Q 35, page 16 |
| Giving gifts | Q 51, page 24 |
| Doing things away from here | Q 53, page 25 |
| Going outside | Q 55, page 26 |
| Watching or listening to TV | Q 65, page 33 |
| Music | Q 69, page 34 |
Using the PELI when an individual is unable to communicate…
What if individuals are unable to communicate their preferences independently? Appendix B – Alternative Ways to Learn About Individual Preferences (pages 7-8) discusses how to explore preferences when people are unable to express them verbally due to cognitive impairment, developmental disabilities or other communication barriers.
Step 2: Integrate Preferences Into Care Plans
Once you’ve gathered information about a person’s daily preferences, the next step is to assure that the care plan reflects and honors the individual’s wishes and strengths. An understanding of what is most important to an individual is crucial to designing and carrying out person-centered care.
To assure that preferences are woven into the care plan:
- Summarize the person’s important preferences and present the information during a care conference.
- Attend the care conference and ask the care team about approaches they can use to honor the individual’s preferences. Brainstorm with them to devise creative solutions when needed.
- Use the PELI to reassess the individual’s preferences quarterly, annually, or when there is a significant change in the person’s physical or mental health, functional status or other circumstances. Be sure to share any new information with the care team.
See Appendix C – Integrating Preferences into the Care Plan (pages 9-10) for more guidance on this step.
Step 3: Communicating Preferences to Enhance Person-Centered Care
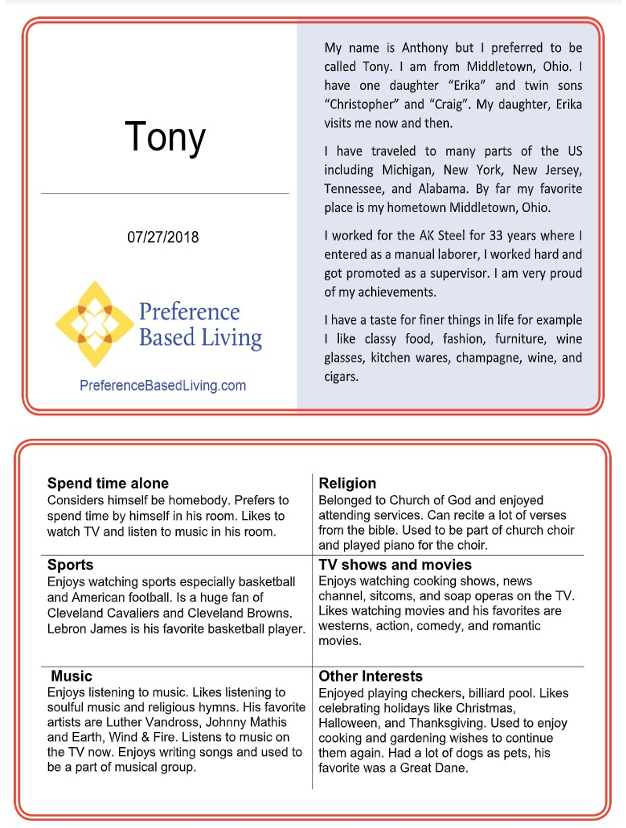
In the press of everyday nursing home life, care teams sometimes find it challenging to convey information about each resident’s key preferences with staff members in other relevant departments as well as across shifts and days. Preferences for Activities and Leisure (PAL) Cards are an easy tool to share information with care team members, volunteers and residents. Based on knowledge gained from the PELI, PAL Cards and provide a profile of the individual’s background and key preferences. Experience shows that PAL Cards promote more personalized care and connection among residents, staff, and volunteers.
Consider asking nursing home staff to create a PAL card for the resident under your guardianship. Find a how-to tip sheet along with sample PAL Cards, downloadable template, and step–by–step video, on the Resources page of our website under PAL Card Resources.
Special Issue: Honoring Preferences when the Choice Involves Risk
Occasionally, residents have important preferences that providers view as “too risky” to fulfill – perhaps a choice for a specific food or activity. In this situation, consider using a process for shared decision-making that respects resident rights for self-determination, while alleviating risks associated with the preference.
To learn about this step-by-step process, check the Resources page of our website for Honoring Preferences When the Choice Involves Risk. There you will find a tip sheet, toolkit, and training video on ways to honor residents’ choices and preferences, while reducing the associated risks.
This section offers tips to prepare for and conduct preference assessment interviews. Also, view our free training video, Interviewing Older Adults Using the PELI (see Resources at PreferenceBasedLiving.com.)
Note: The instructions that follow pertain to individuals who can communicate their preferences verbally. See Appendix B for strategies to use when an individual has cognitive impairment, developmental disabilities or other communication barriers.
Before the Interview
- Familiarize yourself with PELI questions and instructions.
- Print the last page of the PELI, showing response options printed in large font. During the interview, hand the response sheet to the resident.
- Select a comfortable, private setting.
- Sit so that the resident can see your face.
- Make sure the resident can hear you. Residents should use their usual hearing aids or other communication devices. If the resident can’t hear you, try headphones or a hearing amplifier.
Starting the Interview
- Introduce yourself to the individual.
- Describe what you are going to ask the person to do.
- Explain how the interview works, including the response choices and follow up questions.
- When asking detailed questions under each preference item, ask the open-ended question first and write down the resident’s response.
During the Interview
- Be careful not to “put words in the mouth” of the interviewee.
- Give each person time to collect their thoughts and explain their preferences.
- As needed, offer prompts, such as: “Is there anything you’d like to add?” “Can you say more about that?”
- Stop the interview if the individual:
- Becomes fatigued. Offer to pause the interview and return at another time. o Refuses to answer any more questions. Respect the person’s wishes and discontinue the interview.
- Gives more than five “Non-Responses” in a row. Stop the interview and consult instructions in Appendix B on the next page.
At the end of each interview, be sure to thank the individual and let them know that the information you’ve discussed will be used to help plan their care and daily activities. Keep in mind that PELI interviews are meant to be enjoyable conversations and can be completed in more than sitting. Interviews provide a meaningful opportunity to get to know the person, and gather insight that will help the care team provide more individualized care that enhances quality of life.
Studies show that older adults with mild to moderate dementia can report their preferences reliably and consistently. Therefore, we recommend approaching each person three separate times, on different days, before determining that a PELI interview cannot be completed. In this situation, consider the alternatives preferences below to learn about preferences.
Talk with Staff during Visits and Care Planning Meetings
- Ask care team members how the individual responds during daily care and recreational activities.
- If a person frequently seems agitated, depressed or holds back from interaction, these could be signs that their care delivery or activity preferences are not being honored. The team can then explore ways to tailor services to address the individual’s preferences more effectively.
- Talk with the care team about their experiences and observations of the individual’s preferences.
- Staff might have a sense of preferred daily patterns – for example, as when the individual naturally wakes up or wants to go to bed, and emotional reactions to activities throughout the day. You may need to “shadow” direct care staff so they can talk with you while they perform their duties.
- Ask direct care workers about what they have noticed regarding:
- Preferred bathing type (tub bath, shower, bed/sponge bath), time of day and how often to bathe.
- Preferred routines for personal care (when to get up; caring for mouth, hair, nails, bathroom needs; taking a nap, bedtime, clothes to wear).
- Preferences related to staff relationships (the name individual prefers to be called; what seems to help the person feel better when upset; how staff should convey that they care and respect the individual).
- Preferences relating to the environment, such as desired room temperature and lighting; how the bed should be set up for comfort; personal belongings (e.g. doll, stuffed animal, plant); things they wish to take care of.
- Ask direct care workers or dietary staff what, when and where the individual likes to eat, and whether the person likes snacks between meals and wants to be involved in cooking.
- Ask recreation staff about their observations regarding preferences related to:
- Independent pursuit activities, such as reading, listening to music, keeping up with the news, using a computer, watching or listening to TV, participating in favorite hobbies or activities (see the detailed questions in the PELI for examples to prompt staff).
- Activities with others, such as attending entertainment events, watching movies, going outside, taking part in religious services or practices, exercising, playing games, caring for plants, sports, reminiscing, shopping, and being around animals.
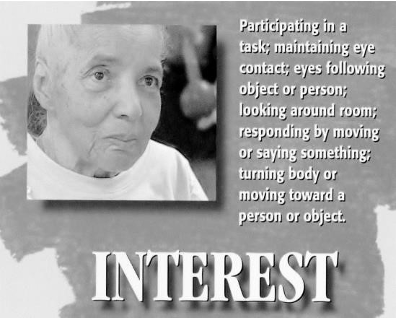
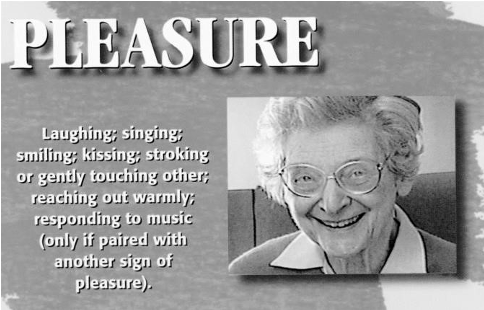
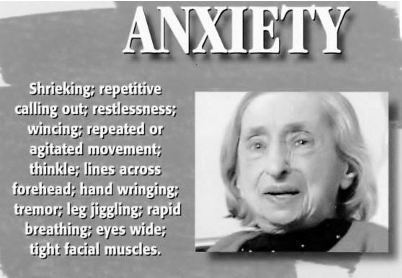
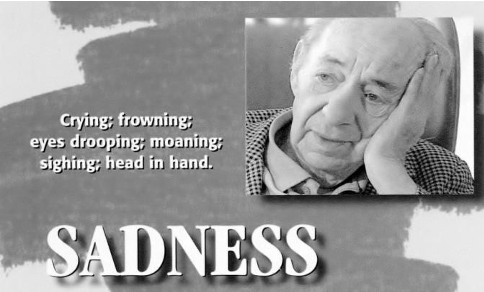
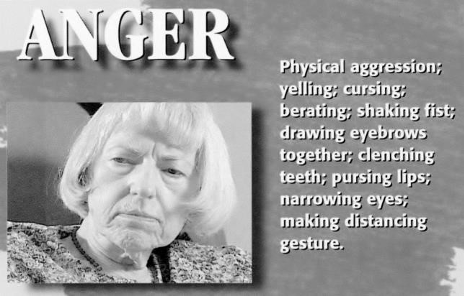
If you can spend time observing the person under your guardianship, you may be able to identify their likes and dislikes. Observing emotion can be highly beneficial in learning the preferences of individuals who can no longer express themselves verbally. Training yourself to look for signs of interest and pleasure or anger and anxiety and even apathy can provide you with valuable information and insight into a person’s preferences.
Likely a preferred activity if you observe the following emotions:
Not likely to be a preferred activity if you observe the following emotions:
Using the Preferences for Everyday Living Inventory (PELI) to personalize care offers important benefits for residents and communities. Understanding and meeting preferences:
- Enhances an individual’s autonomy, quality of life and physical and emotional wellbeing.
- Supports more effective and holistic care planning.
- Increases satisfaction among residents.
- Strengthens trust and communication among residents, guardians, and nursing home staff.
- Complies with regulations requiring that care plans reflect an individual’s voice and preferences so that each person can experience a meaningful and enjoyable life.
How to Prepare for the Care Plan Meeting
Guardians can prepare for care-planning meetings by completing a PELI interview, summarizing the information, and bringing a list of preferences to the meeting. When drafting care plan summaries, we recommend writing in the resident’s voice. For example:
- Personal Care Preferences: Consider my most important preferences, such as choosing what clothes to wear, in order to help me engage positively in care that I can do myself.
- Recreation Preferences: Consider my most important preferences, such as doing my favorite activities — reading, painting and gardening — in order to help me enjoy my leisure time.
Also, during the care-planning meeting, we recommend that you ask about an individual’s behavioral responses during personal care and their level of engagement during recreational activities. Consider asking:
- How frequently does the individual participate in recreational activity?
- Does the person participate independently, in small or large groups, or individually with a recreation assistant?
- How does the person respond to leisure pursuits? Does the person seem to be happy, agitated, actively engaged or observing passively? Is there a verbal or non-verbal response?
Developing Care Plans that Build Dignity, Pride, and Success
Care plans should reflect and honor the individual’s strengths and wishes. The aim is to develop achievable goals that support the individual’s priorities and account for their unique needs, challenges and strengths. Guardians can suggest ways to tailor care delivery for more person-centered results, such as:
- Adapt activities and services to the individual’s interests and functional abilities. Well-crafted care plans can reduce stress, agitation, depression and other signs of discomfort.
- Collaborate with the care team to solve obstacles in meeting preferences. Think creatively and “out of the box” to support the resident’s top preferences and priorities. (Find resources related to Honoring Preferences When the Choice Involves Risk at PreferenceBasedLiving.com.)
As a guardian, keep in mind that you can advocate for members of the care team to follow these approaches.
A Strengths-Based Approach to Build Dignity and Promote Positive Outcomes
| Functional barriers to preferred activities | Strength-based approach | Examples of creative adaptations to encourage participation |
| Physical: Ability to complete task with previous skills has changed. | Use adaptive equipment or approaches | Provide large print or audio books Add raised planters for gardening |
| Cognitive: Frustration with complex tasks due to decreased comprehension or problem solving. | Simplify tasks. Increase individual’s confidence through encouragement and small successes | Offer two outfits to choose from, not three, in order to ease decision making When asking a question, allow more time for the individual to respond |
| Social/Environmental: Prefers privacy and/or quieter environment. | Perform tasks one-to-one or in a small group | Form small groups for individuals with comparable skills or functional levels |
| Social: Difficulty adjusting to a new environment because prior social supports are less available. | Support adjustment and facilitate social interactions | Incorporate personal items into the individuals’ day Introduce client to peers with similar interests and functional levels |
| Mental health/social: High anxiety, diminished ability to manage stress. | Provide support at a slow pace in synch with the individual’s reactions (i.e., monitor for positive or negative response) | Whenever possible, bring preferred activity to individual – for example, large-piece puzzles, picture books related to past history (military service or a love of animals), card games (matching games) adult coloring books with markers. Introduce relaxation exercises, such as yoga, meditation and other techniques Provide opportunities for independent leisure and one-to-one interventions Play familiar music in the comfort of the resident’s own room. Consider the Music and Memory program (see musicandmemory.org/) |
We encourage you to copy and distribute this toolkit, but please include and adhere to the terms of the Creative Commons license: Katherine Abbott, Ph.D. & Kimberly Van Haitsma, Ph.D. This work is licensed under the Creative Commons Attribution-NoDerivatives 4.0 International License. Based on a work at https://preferencebasedliving.com/. To view a copy of this license, visit http://creativecommons.org/licenses/by-nd/4.0/.