Background
- Knowledge of nursing home (NH) residents’ everyday care preferences is foundational in that it allows for the delivery of person-centered care and individualized care planning.
- However, little is known about how integrating preferences into care delivery impact outcomes of care.
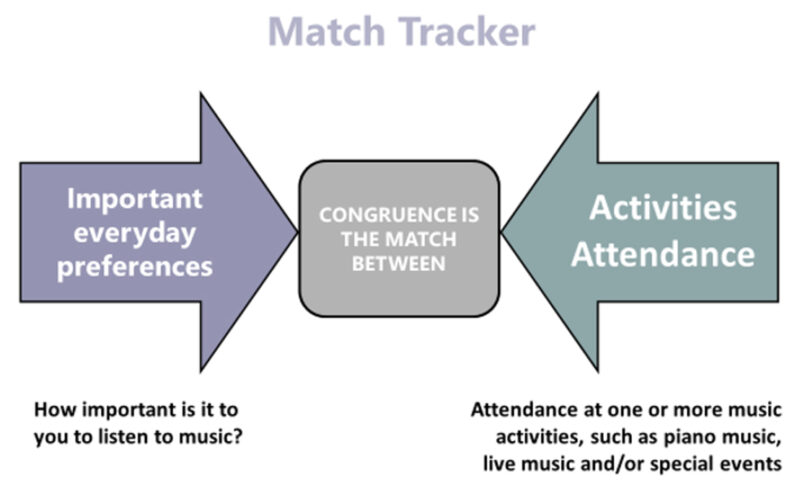
- The Preference Match Tracker is an objective metric that tracks the number of recreation activities NH residents attend that match or are “congruent” with resident important preferences (Heid et al., 2017).
- Here, we explored how Preference Match Tracker data were linked to NH residents’ self-reported pain over the course of one year.
Sample and Data Description
- Data were drawn from the Electronic Medical Records (EMR) of one non-profit, long-term care organization in PA who used Preference Match Tracker data to guide daily care delivery and quality improvement efforts to improve person centered care over 4-years.
- This organization had a history of assessing preferences with the Preferences for Everyday Living (PELI) inventory (Van Haitsma et al., 2016) and aligning activity offerings to residents’ preferences.
- Data were extracted from Jan. 1, 2016, to Mar. 13, 2020 (pre-COVID19) – N = 586 residents
73% Female
24% Married
60% Widowed
99% White
66% Lived in the facility for 90 days or less
77% Medicaid
43% Cognitively Capable
30% Moderately Impaired
27% Severely Impaired
Methods & Analyses
- Resident attendance at activities, as well as activities declined, per week was tracked as a metric for quality improvement in the EMR.
- We aligned the recreational activity attendance data for a given week with the EMR clinical data corresponding to that week from the MDS 3.0.
- 1-year of data were used (Time 0 to Time 4) – each time point about 3 months apart.
- We used PROC GLIMMIX in SAS 9.4, to model repeated measures logistic regression with time as the repeated measure, over 1 year.
- Covariates included age, gender, cognitive ability, length of stay, sensory impairment, and activities of daily living (ADL) functional ability.
- Six key attendance/declining variables were considered:
| 1 | Congruent Attendance: Activity was attended and is congruent (i.e., matches a preference of the resident) |
| 2 | Non-congruent Attendance: Activity was attended and is non-congruent (i.e., does not match a preference of the resident) |
| 3 | Total Attendance: Total number of activities attended regardless of whether they were congruent or non-congruent |
| 4 | Congruent Declined to Attend: Resident declined the invitation to attend an activity that matched the preference of the resident. |
| 5 | Non-congruent Declined to Attend: Resident declined the invitation to attend an activity that did not match the preference of the resident. |
| 6 | Total Declined to Attend: Total number of activities declined regardless of whether they were congruent or non-congruent |
- Pain data were collected from the MDS 3.0 and dichotomously coded as pain or no pain.
| T0 | T1 | T2 | T3 | T4 | |
| % YES (N) | 38% (220) | 29% (165) | 26% (138) | 24% (120) | 21% (100) |
Results
- There were no associations of age, gender, or hearing impairment with pain.
- Reported pain symptoms decreased over one year.

- Individuals reported more pain if they:
Were more cognitively capable
Lived in the nursing home < 90 days
Had better vision

Reported more functional impairment
Were more depressed
Reported a greater # of important preferences for daily living
- After accounting for covariates, attending more congruent recreational activities was associated with less pain over time.
- Only individuals with severe cognitive impairment reported less pain when reporting greater non-congruent attendance.
- Individuals who decline recreational activities more (preferent congruent or non-congruent) also reported less pain.
Discussion
- Activity attendance may be beneficial for pain experience for NH residents with and without dementia, possibly by distracting residents from pain through meaningful engagement.
- Higher attendance, and specifically attendance in preferred, meaningful activities, can support individuals experiencing pain.
- Less reported pain may also promote residents’ capacity for engagement in activities, specifically preferred activities.
- Individuals who decline to attend more activities, may report less pain or individuals with more pain may be invited to attend fewer activities. Future work should explore the directionality of these relationships.
- Future work should explore these associations in additional NH samples and examine the association of preferent congruent attendance and declining with additional objective outcomes (i.e., functional limitations and depressive symptoms).
Acknowledgements
This work has been completed by the Preference Based Living Team with funding from the Alzheimer’s Association’s Advancing Research on Care and Outcome Measurement 3.0 (ARCOM) grant #ARCOM-23-1003207.
For more information:
Kimberly VanHaitsma, ksv110@psu.edu, www.preferencebasedliving.com